Uterine Tumor recovery starts with proven steps. Learn key treatments, lifestyle shifts, and expert-backed strategies to heal and prevent recurrence.
Uterine Tumor: 8 Essential Facts Every Woman Must Know
Understanding Uterine Tumors: Types and Prevalence
Understanding Uterine Tumors: Types and Prevalence
Defining uterine tumors and their common varieties
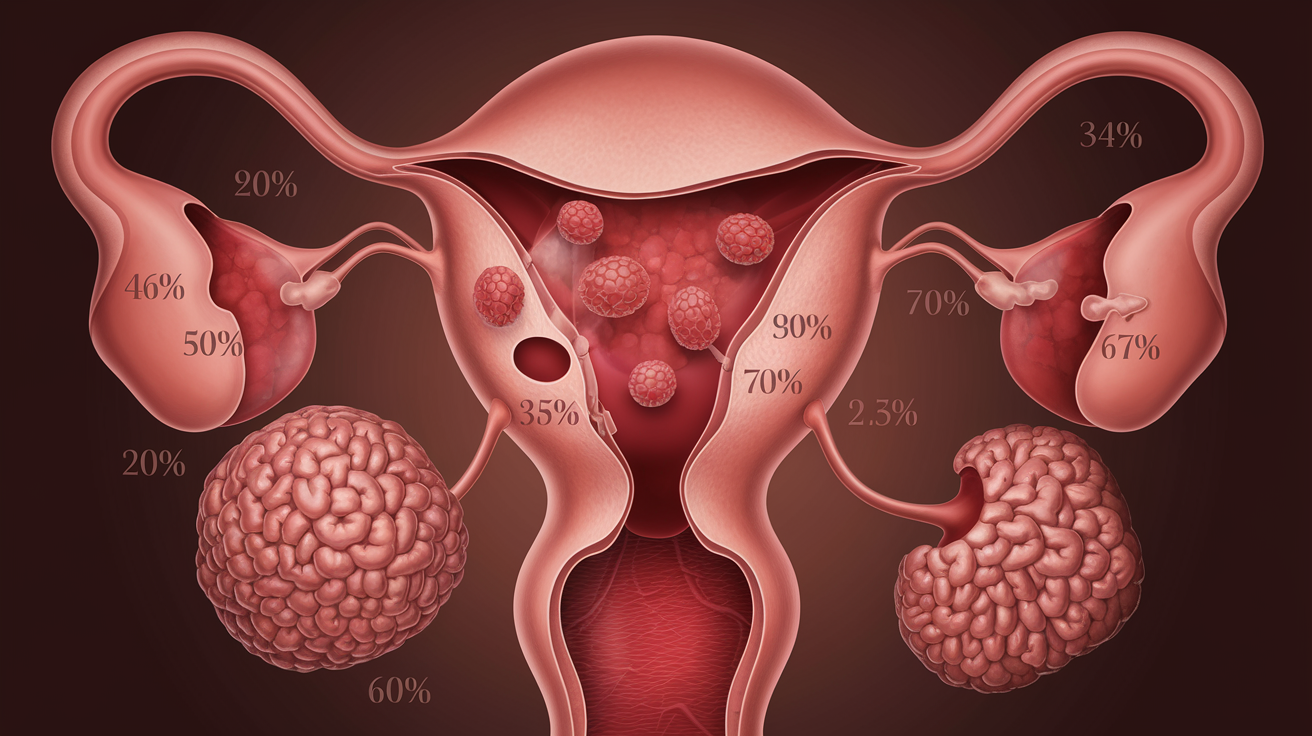
Uterine tumors are abnormal growths that develop in the uterus, the hollow, pear-shaped organ in a woman’s pelvis where fetal development occurs. These growths can vary significantly in size, location, and severity. The most common types include uterine fibroids (leiomyomas), which are non-cancerous growths of the muscle tissue, and endometrial polyps, which are overgrowths of the uterine lining. Less common but more serious are uterine sarcomas and endometrial carcinomas, which are malignant forms of uterine tumors.
Fibroids represent the most prevalent variety, with different classifications based on their location within the uterine wall:
- Submucosal: Growing underneath the inner lining of the uterus
- Intramural: Developing within the muscular wall
- Subserosal: Forming on the outer surface of the uterus
- Pedunculated: Connected to the uterus by a stalk-like growth
How frequently uterine tumors occur across different age groups
Uterine tumors, particularly fibroids, show distinct patterns of prevalence across age groups. Women of reproductive age face the highest risk, with incidence rates increasing significantly from the late 30s through the 40s. Studies indicate that approximately 70-80% of women will develop uterine fibroids by age 50, though many remain asymptomatic and undiagnosed.
The prevalence distribution typically follows this pattern:
- Ages 20-30: Relatively uncommon, affecting less than 20% of women
- Ages 30-40: Moderate prevalence, with approximately 30-40% affected
- Ages 40-50: Peak prevalence, with up to 70-80% affected
- Post-menopause: Risk declines as hormone levels decrease
Malignant uterine tumors, while less common overall, show a different age distribution pattern, with risk increasing significantly after menopause.
Distinguishing between benign and malignant tumors
The distinction between benign and malignant uterine tumors is crucial for proper treatment planning and prognosis. Benign tumors, such as most fibroids, typically grow slowly, don’t invade surrounding tissues, and rarely spread to other parts of the body. They may cause symptoms but are generally not life-threatening.
Malignant uterine tumors, such as endometrial cancer and uterine sarcoma, demonstrate several concerning characteristics:
- Rapid, irregular growth patterns
- Invasion of surrounding tissues
- Potential to metastasize to distant organs
- More severe symptoms including abnormal bleeding and pain
Diagnostic imaging and tissue biopsies are essential for accurately distinguishing between benign and malignant growths, as visual examination alone is insufficient.
Risk profiles: who is most vulnerable to developing uterine tumors
Several factors increase a woman’s vulnerability to developing uterine tumors:
- Genetic predisposition: Family history significantly increases risk, suggesting hereditary components
- Hormonal factors: Higher lifetime exposure to estrogen correlates with increased risk
- Age: Risk increases throughout reproductive years, peaking just before menopause for fibroids
- Race and ethnicity: Studies show higher prevalence and severity among women of African descent
- Lifestyle factors: Obesity, poor diet, and sedentary lifestyle may increase risk
- Medical history: Conditions like hypertension, diabetes, and polycystic ovary syndrome may elevate risk
Understanding these risk profiles helps healthcare providers identify high-risk individuals who may benefit from more vigilant screening and preventive measures.
Now that we’ve established a foundation for understanding what uterine tumors are, their types, and who faces the greatest risk, we’ll explore how to recognize the warning signs in the next section. Early detection through symptom awareness can significantly improve treatment outcomes and quality of life.
Recognizing the Warning Signs
Recognizing the Warning Signs
Now that we understand the different types of uterine tumors and their prevalence among women, it’s crucial to recognize the warning signs that might indicate their presence. Early detection is key to successful treatment and better outcomes.
Early symptoms that should never be ignored
Uterine tumors, particularly uterine cancer, often present with distinct early warning signs that should prompt immediate attention:
- Abnormal vaginal bleeding: This is the most common and significant indicator of potential uterine tumors. Any bleeding that occurs outside your normal menstrual cycle deserves attention.
- Unusual vaginal discharge: Discharge that contains blood, appears in different colors than usual, has a foul odor, or looks purulent (pus-like) could signal a problem.
- Pelvic pain and pressure: Persistent discomfort or a feeling of fullness in your pelvic region may indicate the presence of uterine tumors.
As these conditions progress, you might experience additional symptoms such as:
- Abdominal bloating due to fluid accumulation
- Gastrointestinal issues, including painful bowel movements
- Increased urinary frequency caused by tumor pressure on the bladder
- Unintentional weight loss resulting from decreased appetite
Distinguishing tumor symptoms from normal menstrual discomfort
Many women experience discomfort during their menstrual cycles, making it challenging to differentiate between normal period pain and warning signs of uterine tumors. Here’s how to tell the difference:
- Timing of bleeding: Normal menstrual bleeding follows a predictable pattern, whereas tumor-related bleeding often occurs between periods, after intercourse, or after menopause.
- Duration and intensity: While some heavy periods are normal, unusually heavy or prolonged bleeding that soaks through multiple pads or tampons in a short time is concerning.
- Consistency of symptoms: Menstrual discomfort typically follows a cyclical pattern, while tumor symptoms tend to persist or worsen over time.
It’s particularly important for menopausal women to be vigilant. If you’ve gone through menopause, any vaginal bleeding should be considered abnormal and warrants immediate medical attention.
When to seek immediate medical attention
Given the importance of early detection, certain symptoms should prompt you to seek medical care without delay:
- Any post-menopausal bleeding: Even light spotting after menopause is abnormal and requires evaluation.
- Persistent abnormal bleeding: Bleeding between periods or unusually heavy periods that continue for several cycles.
- Progressive symptoms: If you notice your symptoms are getting worse or new symptoms are developing, don’t wait to consult with your healthcare provider.
- Concerning discharge: Any discharge that is unusual in color, consistency, or odor, especially if accompanied by other symptoms.
The good news is that most uterine cancers reveal symptoms before advancing to critical stages. This early warning system gives you the opportunity to seek prompt medical attention, which significantly enhances the likelihood of successful treatment.
With these warning signs in mind, next, we’ll explore what you can expect during the diagnosis process. Understanding how healthcare providers evaluate these symptoms will help you navigate the sometimes complex journey of medical testing with greater confidence and less anxiety.
Diagnosis Process: What to Expect

Diagnosis Process: What to Expect
Now that we’ve covered the warning signs of uterine tumors, understanding how these conditions are diagnosed is crucial for early intervention. After noticing symptoms and consulting your doctor, you’ll enter a structured diagnostic process designed to accurately identify the nature of any uterine abnormalities.
Initial screening methods your doctor may recommend
Your diagnostic journey typically begins with a thorough physical and pelvic examination. During this examination, your doctor will use two fingers inserted into the vagina while pressing on your abdomen to feel the uterus and ovaries for any abnormalities or unusual growths.
Following the physical examination, imaging tests are often the next step. A transvaginal ultrasound is commonly used as an initial screening tool. This procedure uses sound waves to create detailed images of your pelvic organs, helping doctors assess the thickness and texture of the endometrium while ruling out other conditions. This non-invasive procedure is particularly helpful in identifying uterine fibroids and evaluating endometrial thickness.
Pelvic ultrasounds may also be recommended, providing a broader view of the reproductive organs and surrounding structures. These initial screening methods are crucial in determining whether further investigation is necessary.
Advanced diagnostic techniques and their accuracy
If initial screenings suggest abnormalities, your healthcare provider may recommend more advanced diagnostic procedures. Hysteroscopy is one such technique that involves inserting a thin, lighted instrument into the uterus, allowing for direct visualization of the uterine cavity. This procedure is particularly effective at identifying issues within the endometrium.
When a uterine tumor is suspected, tissue sampling becomes essential. An endometrial biopsy involves removing a small tissue sample from the uterine lining for microscopic examination. In cases where sufficient tissue cannot be obtained through a standard biopsy, a dilation and curettage (D&C) procedure may be performed. This involves dilating the cervix and scraping tissue from the uterine lining for examination.
For more comprehensive staging and evaluation, additional imaging studies may be recommended:
- CT scans
- MRI scans
- PET scans
These advanced imaging techniques help determine if cancer has spread beyond the uterus. Blood tests, including advanced genomic testing and the CA-125 test, can provide additional information about potential cancer presence and aid in treatment planning.
Questions to ask your healthcare provider during diagnosis
Being an active participant in your diagnosis process empowers you to make informed decisions. Consider asking your healthcare provider:
- What specific type of uterine tumor do you suspect?
- What diagnostic tests will I need, and why?
- How should I prepare for each procedure?
- What are the risks associated with each diagnostic test?
- How long will it take to receive the results?
- Will I need someone to drive me home after the procedures?
- What post-procedure care instructions should I follow?
Documenting your symptoms and questions before appointments can help ensure you receive the most accurate diagnosis possible.
Understanding your diagnostic results
After completing diagnostic procedures, your healthcare provider will explain the findings. If cancer is diagnosed, it will be classified by stage, ranging from stage 1 (confined to the uterus) to stage 4 (spread to distant organs).
For uterine fibroids or benign tumors, your doctor will discuss size, location, and number of growths, as these factors influence treatment recommendations. Understanding your diagnostic results is crucial for making informed decisions about treatment options.
With a clear understanding of your diagnosis, you’ll be better prepared to explore the various treatment options available. In the next section, we’ll discuss the comprehensive treatment approaches for uterine tumors, from surgical interventions to non-invasive therapies designed to preserve your reproductive health and quality of life.
Treatment Options Explained

Treatment Options Explained
Now that we understand how uterine tumors are diagnosed through procedures like pelvic exams, imaging tests, and biopsies, let’s explore the various treatment options available to patients facing this diagnosis.
A. Non-surgical approaches for managing uterine tumors
For many women, particularly those with less severe conditions or those who wish to preserve fertility, non-surgical approaches can be effective. Radiation therapy is one such option, which can be administered either externally or internally to target cancer cells. External radiation delivers beams from outside the body, while internal radiation (brachytherapy) places radioactive materials directly in or near the tumor site.
Chemotherapy is another non-surgical approach, using powerful drugs to kill cancer cells. This treatment is typically reserved for more advanced cases or when cancer has spread beyond the uterus. For hormone-sensitive tumors, hormone therapy may be recommended to block or reduce hormones that can stimulate cancer growth.
Newer approaches include targeted therapies, which attack specific mechanisms within cancer cells, and immunotherapies, which boost the body’s natural immune response against cancer cells. These treatments often have fewer side effects than traditional chemotherapy.
B. Surgical interventions and their effectiveness
Surgery remains the cornerstone of treatment for many uterine tumors. The most common surgical procedure is a hysterectomy, which involves the removal of the uterus. In many cases, this also includes removing the fallopian tubes and ovaries (a procedure known as bilateral salpingo-oophorectomy).
For comprehensive staging and treatment, surgeons may also remove lymph nodes to check for cancer spread. The effectiveness of surgical intervention is generally high, particularly for early-stage cancers confined to the uterus. Complete removal of the affected organs often results in a cure when the cancer hasn’t spread.
C. Emerging therapies showing promise
Research continues to advance the field of uterine tumor treatment. Clinical trials at institutions like the Mayo Clinic investigate new approaches to target cancer cells more effectively while minimizing damage to healthy tissue. Palliative care therapies are also evolving, focusing not just on managing the cancer itself but improving quality of life during treatment by addressing symptoms and side effects.
D. How to choose the right treatment pathway for your situation
Choosing the right treatment requires careful consideration of several factors. Your doctor will consider the stage and grade of your tumor, your overall health, and whether you wish to preserve fertility. Personal preferences and quality of life concerns should also guide your decision.
It’s important to prepare thoroughly for medical appointments by documenting symptoms and questions. Many patients find it helpful to seek second opinions and to understand all available options before making decisions. Your healthcare team should provide comprehensive information about benefits, risks, and expected outcomes of each treatment option.
E. Recovery expectations for different treatment methods
Recovery varies significantly depending on the treatment method chosen. Surgical procedures like hysterectomy typically require several weeks of recovery time, with restrictions on physical activity. Side effects may include pain, fatigue, and hormonal changes if the ovaries are removed.
Non-surgical treatments have their own recovery profiles. Radiation therapy may cause fatigue and skin changes, while chemotherapy can lead to nausea, hair loss, and increased susceptibility to infection. Hormone therapy may cause menopausal symptoms even in pre-menopausal women.
Throughout recovery, maintaining a support system is crucial. Patients are encouraged to engage in their usual activities as much as possible and to communicate openly with their healthcare team about any concerns or side effects.
As we transition to discussing the impact of uterine tumors on reproductive health in the next section, it’s important to note that treatment choices often directly affect fertility and reproductive function. The decisions made during this treatment phase will significantly influence future reproductive options, making it essential to discuss these concerns openly with your healthcare team.
Impact on Reproductive Health

Impact on Reproductive Health
Now that we’ve explored the various treatment options for uterine tumors, it’s crucial to understand how these growths and their treatments can affect your reproductive health. For many women, fertility concerns become a significant consideration when facing a uterine tumor diagnosis.
Fertility considerations for women with uterine tumors
Uterine fibroids, the most common type of uterine tumors, have a complex relationship with fertility. While many women with fibroids can successfully conceive, these benign growths may contribute to infertility in approximately 2-3% of cases. The impact on fertility largely depends on the location of the fibroids:
- Submucosal fibroids: These tumors, which protrude into the uterine cavity, are most detrimental to fertility. Research shows they are associated with lower pregnancy and live birth rates, as they can directly interfere with embryo implantation.
- Intramural fibroids: These growths within the uterine wall have variable effects on fertility, particularly when they’re 5 cm or larger.
- Subserosal fibroids: Located on the outer surface of the uterus, these typically don’t affect fertility outcomes.
If you’re experiencing difficulty conceiving, it’s essential to consult with a reproductive endocrinologist. They can help determine whether your fibroids are a contributing factor or if other infertility issues might be present.
Pregnancy possibilities after diagnosis and treatment
The good news is that pregnancy remains possible for many women with uterine tumors, even after treatment. Following a myomectomy (surgical removal of fibroids while preserving the uterus), fertility outcomes often improve, especially when submucosal fibroids have been removed.
However, pregnancy with fibroids does come with some considerations:
- Increased risk of premature birth
- Higher likelihood of cesarean section delivery
- Slightly elevated risk of miscarriage
- Possible fibroid growth during pregnancy due to hormonal changes
During pregnancy, collaborative care between your obstetrician and specialists is crucial to monitor fibroid changes and address any complications. While most women with fibroids can achieve a natural birth, statistics show a significantly higher rate of C-sections among those with fibroids.
Family planning options to discuss with your healthcare team
When diagnosed with uterine tumors, several family planning discussions should occur with your healthcare team:
- Timing of treatment: If you’re planning to conceive in the near future, discuss the optimal timing for treatment. In some cases, addressing symptomatic fibroids before attempting pregnancy may improve outcomes.
- Fertility preservation: Consider fertility preservation options like egg freezing, especially if treatments might affect your future fertility. This is particularly relevant if you’re not ready for pregnancy but want to maintain the option for the future.
- Myomectomy approaches: If surgery is recommended, discuss the various surgical approaches for myomectomy, including minimally invasive options. The surgical technique may impact recovery time and future pregnancy outcomes.
- Fertility treatments: For those struggling to conceive, fertility treatments can still be pursued with fibroids present, though your doctor may recommend removing certain types of fibroids first to improve success rates.
- Post-pregnancy considerations: Be aware that while some fibroids may regress after pregnancy, others can persist and potentially cause ongoing symptoms that might require further treatment.
With proper medical guidance, many women with uterine tumors can fulfill their family planning goals. Your healthcare team can develop a personalized approach based on your specific situation, tumor characteristics, and reproductive desires.
As we consider the impact of uterine tumors on reproductive health, it’s equally important to focus on living well despite this diagnosis, which we’ll explore in the next section.
Living Well Despite Diagnosis

Living Well Despite Diagnosis
Now that we’ve explored how uterine tumors can affect your reproductive health, it’s equally important to understand how to maintain quality of life after diagnosis. Whether you’re dealing with uterine fibroids or a more serious condition, implementing effective coping strategies can make a significant difference in your recovery journey.
Managing Physical Symptoms Effectively
Physical symptoms from uterine tumors and their treatments can be challenging, but several approaches can help minimize discomfort:
- Nutrition modifications: Embrace a balanced diet rich in fruits, vegetables, whole grains, and lean proteins to support overall health and recovery
- Hydration: Maintain adequate fluid intake throughout the day
- Dietary adjustments: Limit processed foods that may exacerbate inflammation and discomfort
- Regular physical activity: Engage in moderate exercise as approved by your healthcare provider to manage fatigue and improve overall wellbeing
- Consistent sleep schedule: Establish regular sleep patterns to enhance recovery and energy levels
These lifestyle modifications can help manage treatment side effects while supporting your body’s natural healing processes.
Emotional Wellness Strategies Following Diagnosis
A uterine tumor diagnosis affects not just your physical health but emotional wellbeing too. Consider these approaches:
- Mindfulness practices: Incorporate mindful breathing, guided imagery, and meditation into your daily routine
- Stress reduction techniques: Learn specific methods to calm your mind during difficult moments
- Establishing routines: Create consistent daily patterns that include time for self-care and relaxation
- Recognizing emotional triggers: Become aware of situations that may intensify anxiety about your condition
- Cultivating resilience: Focus on developing a positive mental outlook despite challenges
These techniques can help you navigate the complex emotions that often accompany living with uterine tumors.
Building a Supportive Healthcare Team
Having the right professional support is crucial when managing a uterine tumor diagnosis:
- Seek professional help: Consider therapy or counseling to process emotions related to your diagnosis
- Recognize when you need additional support: Watch for signs like persistent sadness or overwhelming anxiety
- Connect with support groups: Join communities of women experiencing similar health challenges
- Communicate openly with healthcare providers: Ensure all your concerns are addressed during appointments
- Coordinate care: Work with specialists who understand your specific type of uterine tumor
A comprehensive healthcare team can provide both medical expertise and emotional guidance throughout your journey.
Lifestyle Adjustments That Support Healing
Making thoughtful changes to your daily life can significantly impact your recovery:
- Create a healing environment: Organize your living space to minimize stress and maximize comfort
- Adjust work schedules: Consider flexible arrangements during treatment periods
- Delegate responsibilities: Allow others to help with daily tasks when needed
- Set realistic expectations: Understand that recovery is a process that takes time
- Celebrate small victories: Acknowledge improvements and positive milestones along the way
These adjustments can create space for healing while maintaining as much normalcy as possible in your life.
With these strategies in place for living well despite your diagnosis, you’ll be better positioned to focus on preventive measures. In the next section, we’ll explore preventive approaches worth adopting to minimize complications and support long-term health while living with uterine tumors.
Preventive Measures Worth Adopting

Preventive Measures Worth Adopting
Now that we’ve explored how to live well despite a uterine tumor diagnosis, let’s focus on something equally important: prevention. While not all uterine tumors can be prevented, research indicates several evidence-based strategies that can significantly reduce your risk.
Evidence-based strategies to reduce tumor risk
Weight management stands as one of the most powerful preventive measures against uterine tumors, particularly endometrial cancer. The rising prevalence of endometrial cancer has been closely linked to the obesity epidemic, with obesity implicated in approximately 60% of cases in Europe. Research shows that not only obesity itself but also weight cycling and weight gain during middle age contribute to increased risk.
For women struggling with obesity, bariatric surgery presents a significant protective measure, potentially reducing endometrial cancer risk by an impressive 81% when normal weight is achieved and maintained. This dramatic reduction underscores the importance of addressing obesity as a primary prevention strategy.
Hormonal interventions also play a crucial role in risk reduction. Combined oral contraceptives offer long-lasting protection against endometrial cancer. Similarly, the levonorgestrel intrauterine system (LNG-IUS) has demonstrated protective effects. Newer hormone replacement therapies combining estradiol with bazedoxifene show promise in protecting the endometrium while managing menopausal symptoms.
Physical activity deserves special mention as a key preventive measure. Regular exercise helps maintain healthy weight and may directly reduce cancer risk through multiple physiological mechanisms. Interestingly, dietary choices such as increased coffee and green tea consumption may also contribute to lower risk of uterine tumors.
Screening recommendations by age group
For most women, routine screening for uterine tumors isn’t recommended unless symptoms appear. However, for high-risk groups, particularly those with Lynch syndrome, specialized surveillance programs are vital. These hereditary conditions significantly increase lifetime risk of endometrial and other cancers.
Women with Lynch syndrome should consider more aggressive preventive approaches, including risk-reducing surgeries after completing their families. For these high-risk individuals, regular transvaginal ultrasounds and endometrial biopsies may be recommended starting in their 30s or 40s.
Women with polycystic ovary syndrome (PCOS) represent another high-risk group requiring vigilant monitoring. The hormonal imbalances associated with PCOS increase susceptibility to endometrial abnormalities and should prompt more frequent screening.
The role of regular gynecological check-ups
Regular gynecological exams play a crucial role in early detection and prevention of uterine tumors. These appointments provide opportunities for healthcare providers to assess risk factors, discuss preventive strategies, and identify warning signs that warrant further investigation.
During these visits, physicians can also recommend appropriate preventive interventions based on individual risk profiles. For instance, women taking tamoxifen for breast cancer treatment face increased endometrial cancer risk and require specialized monitoring protocols.
Future preventive approaches may include chemoprevention agents currently under investigation. Research is exploring the potential benefits of medications like aspirin, bisphosphonates, and metformin in reducing uterine tumor risk. These studies aim to identify women at highest risk who might benefit most from targeted interventions.
As we move forward to navigating your healthcare journey, remember that prevention remains your most powerful tool against uterine tumors. By implementing these evidence-based strategies and maintaining regular check-ups, you can significantly reduce your risk while ensuring early detection of any abnormalities that may develop. Your healthcare provider will be your essential partner in developing a personalized prevention plan based on your specific risk factors, age, and health history.
Lifestyle and supportive care play a vital role in managing uterine tumors and improving overall well-being. Here’s how:
1. Diet & Exercise for Recovery
- Anti-inflammatory Foods – Include leafy greens, berries, turmeric, and healthy fats to help reduce inflammation.
- Balanced Nutrition – A diet rich in fiber and lean proteins supports healing and hormonal balance.
- Regular Movement – Activities like yoga, walking, and strength training can improve circulation and mood.
- Weight Management – Maintaining a healthy weight reduces stress on the reproductive system.
2. Pain Management Strategies
- Medications – Nonsteroidal anti-inflammatory drugs (NSAIDs) and prescribed pain relievers help manage discomfort.
- Heat Therapy – Warm compresses or heating pads can soothe pelvic pain.
- Acupuncture & Physical Therapy – Some find relief through holistic approaches like acupuncture or specialized physiotherapy.
3. Psychological & Emotional Support
- Therapy & Counseling – Professional guidance helps in coping with diagnosis and treatment stress.
- Support Groups – Connecting with others facing similar challenges provides emotional relief and encouragement.
- Mindfulness & Stress Reduction – Practices like meditation and deep breathing can ease anxiety and promote healing.
Prioritizing lifestyle changes alongside medical treatment improves quality of life and fosters a sense of control over health.
Navigating Your Healthcare Journey

Navigating Your Healthcare Journey
Now that we’ve explored preventive measures that can help reduce your risk of uterine tumors, let’s focus on how to effectively navigate your healthcare journey if you’ve been diagnosed. Managing uterine tumors requires not only medical treatment but also understanding how to access appropriate care and support throughout your journey.
Insurance and Financial Considerations
Dealing with uterine tumors can create significant financial challenges alongside health concerns. Fortunately, organizations like CancerCare offer financial assistance programs for eligible families coping with cancer-related expenses. These programs can help ease the burden of treatment costs, medication expenses, and other financial challenges that arise during your healthcare journey.
Before beginning treatment, it’s advisable to:
- Contact your insurance provider to understand your coverage for uterine tumor treatments
- Inquire about financial assistance programs through organizations like CancerCare
- Discuss payment plans or financial aid options with your healthcare provider’s billing department
CancerCare’s resource navigation services can help you overcome barriers to care, including identifying programs that might assist with insurance issues or treatment costs.
Finding Specialized Care Providers
Working with specialists who have extensive experience treating uterine tumors can significantly impact your treatment outcomes. Organizations like SHARE and CancerCare emphasize the importance of finding a gynecologic oncologist – a physician who specializes in cancers of the female reproductive system.
When seeking specialized care:
- Ask for referrals to gynecologic oncologists from your primary care doctor
- Utilize patient navigation services offered by organizations like SHARE, which can help connect you with appropriate specialists
- Consider seeking second opinions for complex cases or when multiple treatment options exist
SHARE provides personalized patient navigation specifically designed to address healthcare challenges during treatment for uterine cancer, helping you identify and connect with the most appropriate care providers for your specific situation.
Patient Advocacy Resources and Support Groups
Connecting with others who understand your experience can provide invaluable emotional support and practical advice. Both SHARE and CancerCare offer robust support systems for women dealing with uterine tumors.
Key resources include:
- Support groups facilitated by oncology social workers at CancerCare
- SHARE’s Uterine Cancer Support community with specific programs tailored for patients
- Virtual workshops in both English and Spanish through CancerCare
- The Foundation for Women’s Cancer, recommended as an additional resource
SHARE encourages subscribing to their Uterine Cancer Support email list to receive updates about programs and newsletters. They also host regular events such as webinars focused on gynecologic cancer and fitness classes designed for patients.
For emotional support, CancerCare offers counseling with oncology social workers, accessible via phone at 800-813-HOPE or through email at info@cancercare.org.
Questions to Guide Treatment Decisions
Making informed decisions about your treatment requires asking the right questions and gathering reliable information.
Important questions to consider when making treatment decisions include:
- What are all available treatment options for my specific type of uterine tumor?
- What are the potential side effects and long-term implications of each treatment?
- How might different treatments impact my reproductive health and overall quality of life?
- Are there clinical trials I might qualify for?
Educational resources that can help inform these discussions include:
- CancerCare’s Connect Education Workshops featuring expert insights on current cancer-related topics
- Podcasts covering significant themes like treatment options and research developments
- SHARE’s content library featuring webinars and educational materials specific to uterine cancer
- “Ask CancerCare” feature allowing patients to submit questions directly to experts
By utilizing these resources and support systems, you can become an empowered participant in your healthcare journey, making informed decisions while receiving the emotional and practical support needed throughout your treatment for uterine tumors.
Black Ginger: 10 Essential Benefits for Ultimate Wellness
Share this content: