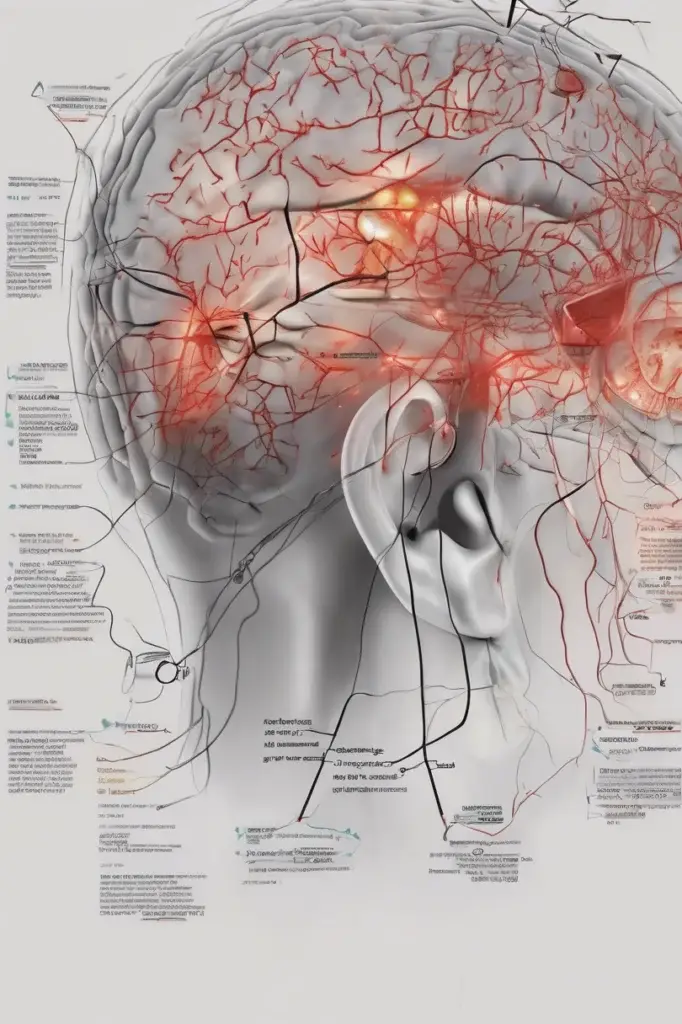
Head ache warning signs: Learn about 5 alarming symptoms beyond stress that hurt your eyes and require urgent attention
Understanding Head Ache Causes
Do you ever experience a throbbing **head ache** that seems to radiate directly from your eyes? Most people brush it off as stress or eye strain, but sometimes, it can be a sign of something more serious. While stress is a common trigger for headaches, especially tension headaches, dismissing recurring or severe headaches with eye pain can be risky. This article will explore five alarming signs that your head ache and eye pain might indicate a condition requiring medical attention. Let's dive in! 🤿
## Introduction: Beyond the Ordinary Head Ache
Headaches are a common ailment, affecting almost everyone at some point in their lives. We often attribute them to factors like:
* Stress at work 😫
* Lack of sleep 😴
* Dehydration 💧
* Staring at screens for too long 💻
However, when a head ache is consistently accompanied by eye pain or visual disturbances, it's crucial to consider other potential causes. Ignoring these symptoms can lead to delayed diagnosis and treatment of underlying conditions. It's important to distinguish between a simple tension head ache and a head ache that signals a more significant health concern.
> "Ignoring recurring headaches with eye pain can lead to delayed diagnosis and treatment of underlying conditions."
This article provides information on five alarming signs associated with head aches and eye pain. It aims to empower you to recognize these warning signals and seek appropriate medical attention. It is not intended as a substitute for professional medical advice. Always consult with a qualified healthcare provider for diagnosis and treatment of any medical condition.
## 1. Glaucoma: The Silent Thief of Sight 👁️
Glaucoma is a group of eye diseases that damage the optic nerve, which connects the eye to the brain. Often, glaucoma develops slowly and without noticeable symptoms, earning it the nickname "the silent thief of sight." However, in some cases, particularly with **acute angle-closure glaucoma**, the onset can be sudden and dramatic, causing severe eye pain, head ache, and blurred vision.
### Understanding Angle-Closure Glaucoma
Angle-closure glaucoma occurs when the iris (the colored part of your eye) blocks the drainage angle, preventing fluid from flowing out of the eye. This leads to a rapid increase in intraocular pressure (IOP), the pressure inside the eye.
### Symptoms of Acute Angle-Closure Glaucoma
The symptoms of acute angle-closure glaucoma can be quite alarming and require immediate medical attention. These may include:
* **Severe eye pain:** A sharp, intense pain in one or both eyes.
* **Head ache:** Often localized around the forehead or temples.
* **Blurred vision:** Sudden onset of blurry or hazy vision.
* **Halos around lights:** Seeing colored rings or halos around lights.
* **Nausea and vomiting:** These symptoms can sometimes accompany the severe pain.
* **Redness of the eye:** The white part of the eye may appear red and inflamed.
### Why It's an Emergency
Acute angle-closure glaucoma is a medical emergency because the elevated IOP can quickly damage the optic nerve, leading to permanent vision loss. If you experience these symptoms, seek immediate medical attention at an emergency room or ophthalmologist's office.
7 Essential Asanas for Stability: Mastering the Art of Balance
### Diagnosis and Treatment
An ophthalmologist can diagnose angle-closure glaucoma by measuring your IOP and examining the drainage angle of your eye. Treatment typically involves medications to lower IOP and a laser procedure called iridotomy, which creates a small hole in the iris to allow fluid to drain properly.
**Table: Comparing Different Types of Glaucoma**
| Type of Glaucoma | Onset | Symptoms | IOP Increase |
| ------------------------- | --------- | ------------------------------------------------------------------------------------------------------------- | ------------ |
| Open-Angle Glaucoma | Gradual | Often asymptomatic in early stages; gradual vision loss | Moderate |
| Angle-Closure Glaucoma | Sudden | Severe eye pain, head ache, blurred vision, halos around lights, nausea, vomiting, red eye | Rapid & High |
| Normal-Tension Glaucoma | Gradual | Similar to open-angle glaucoma, but with normal IOP | Normal |
| Congenital Glaucoma | At birth | Excessive tearing, light sensitivity, cloudy cornea | High |
## 2. Migraine with Aura: A Neurological Storm ⛈️
Migraines are severe head aches that can cause throbbing pain or a pulsing sensation, usually on one side of the head. They are often accompanied by other symptoms, such as nausea, vomiting, and extreme sensitivity to light and sound. Some people experience migraines with aura, which involves visual disturbances or other neurological symptoms that precede the head ache.
### Understanding Migraine Aura
Aura typically develops gradually over 5-20 minutes and lasts for less than an hour. The most common type of aura is visual, but it can also involve sensory, motor, or speech disturbances.
### Common Visual Aura Symptoms
* **Flashing lights:** Seeing bright, shimmering lights or zigzag lines.
* **Blind spots:** Experiencing temporary areas of vision loss.
* **Tunnel vision:** A narrowing of the visual field.
* **Distorted vision:** Objects appearing larger, smaller, or closer than they actually are.
### Head Ache and Eye Pain with Migraine
The head ache associated with migraine can be intense and debilitating. It is often described as a throbbing or pulsating pain that is worsened by physical activity. Eye pain is also a common symptom of migraine, and it can be felt behind the eye, around the eye, or in the eye itself.
### Differentiating Migraine from Other Head aches
While other types of head aches, such as tension head aches, can also cause eye pain, migraines are typically more severe and are accompanied by other symptoms like nausea, vomiting, and sensitivity to light and sound. The presence of aura is also a key differentiator.
**Table: Migraine vs. Tension Head Ache**
| Feature | Migraine | Tension Head Ache |
| ------------------- | ---------------------------------------- | ---------------------------------------- |
| Pain | Throbbing, pulsating, often one-sided | Dull, aching, often both sides |
| Severity | Moderate to severe | Mild to moderate |
| Aura | May be present | Absent |
| Nausea/Vomiting | Common | Uncommon |
| Light/Sound Sensitivity | Common | May be present, but less severe |
| Duration | 4-72 hours | 30 minutes to several hours |
### When to See a Doctor
If you experience frequent or severe migraines, or if your migraines are accompanied by new or unusual symptoms, it's important to see a doctor. They can help you determine the cause of your migraines and develop a treatment plan to manage your symptoms. A neurologist can be particularly helpful in diagnosing and managing migraines.
### Treatment Options
Treatment options for migraines include:
* **Pain relievers:** Over-the-counter or prescription pain relievers can help to relieve migraine pain.
* **Triptans:** These medications are specifically designed to treat migraines and can help to relieve pain and other symptoms.
* **Preventive medications:** If you experience frequent migraines, your doctor may prescribe preventive medications to reduce the frequency and severity of your attacks.
* **Lifestyle changes:** Certain lifestyle changes, such as getting enough sleep, managing stress, and avoiding trigger foods, can also help to prevent migraines.
> "Migraines are more than just bad headaches; they are a neurological condition that can significantly impact quality of life."
## 3. Optic Neuritis: Inflammation of the Optic Nerve 🔥
Optic neuritis is an inflammation of the optic nerve, the nerve that transmits visual information from the eye to the brain. This inflammation can disrupt the nerve's ability to function properly, leading to vision loss, eye pain, and other symptoms.
### Causes of Optic Neuritis
The exact cause of optic neuritis is often unknown, but it is thought to be related to autoimmune disorders, infections, or other inflammatory conditions. Some of the known causes and associated conditions include:
* **Multiple sclerosis (MS):** Optic neuritis is often one of the first symptoms of MS.
* **Infections:** Viral or bacterial infections, such as Lyme disease or measles, can sometimes trigger optic neuritis.
* **Autoimmune disorders:** Conditions like lupus and sarcoidosis can also be associated with optic neuritis.
### Symptoms of Optic Neuritis
The symptoms of optic neuritis can vary depending on the severity of the inflammation and the extent of nerve damage. Common symptoms include:
* **Eye pain:** Pain is often worse with eye movement.
* **Vision loss:** This can range from mild blurring to complete blindness in one eye.
* **Reduced color vision:** Colors may appear washed out or less vibrant.
* **Visual field defects:** Blind spots or areas of vision loss in the visual field.
* **Flashing lights:** Seeing flashing lights or phosphenes.
### Diagnosis and Treatment
An ophthalmologist or neurologist can diagnose optic neuritis by performing a thorough eye exam and neurological evaluation. This may include:
* **Visual acuity testing:** Measuring your ability to see clearly at different distances.
* **Visual field testing:** Assessing your peripheral vision.
* **Color vision testing:** Evaluating your ability to distinguish between different colors.
* **Optical coherence tomography (OCT):** Imaging the optic nerve to assess its structure.
* **Magnetic resonance imaging (MRI):** Imaging the brain and optic nerve to look for signs of inflammation or other abnormalities.
Treatment for optic neuritis typically involves corticosteroids, which can help to reduce inflammation and speed up recovery. In some cases, intravenous immunoglobulin (IVIG) therapy may be used.
### Prognosis
The prognosis for optic neuritis varies depending on the underlying cause and the severity of the inflammation. Many people recover most or all of their vision within a few months, but some may experience permanent vision loss.
**Table: Key Differences Between Optic Neuritis and Glaucoma**
| Feature | Optic Neuritis | Glaucoma |
| ------------------ | ---------------------------------------- | ---------------------------------------- |
| Cause | Inflammation of the optic nerve | Damage to the optic nerve, often due to high IOP |
| Onset | Typically rapid | Usually gradual |
| Eye Pain | Common, especially with eye movement | Uncommon, except in acute angle-closure |
| Vision Loss | Can be significant and rapid | Typically gradual and peripheral |
| Color Vision | Often affected | Usually not affected until late stages |
| IOP | Usually normal | Often elevated, especially in angle-closure |
## 4. Giant Cell Arteritis (Temporal Arteritis): Inflammation of Arteries 💥
Giant cell arteritis (GCA), also known as temporal arteritis, is an inflammation of the lining of the arteries, most often the arteries in the head, especially those in the temples. This inflammation can reduce blood flow to the brain, eyes, and other organs, leading to serious complications.
### Symptoms of Giant Cell Arteritis
The symptoms of GCA can vary, but common signs include:
* **Severe head ache:** Often a throbbing or aching pain in the temples.
* **Scalp tenderness:** Pain or tenderness when touching the scalp.
* **Jaw pain:** Pain when chewing, also known as jaw claudication.
* **Vision problems:** Blurred vision, double vision, or sudden vision loss.
* **Eye pain:** Pain in or around the eyes.
* **Fatigue:** Feeling tired and weak.
* **Fever:** A low-grade fever.
* **Muscle aches:** Pain and stiffness in the shoulders, neck, or hips (polymyalgia rheumatica).
### Why It's a Medical Emergency
GCA can lead to serious complications, including:
* **Permanent vision loss:** Inflammation of the arteries that supply blood to the optic nerve can cause irreversible damage.
* **Stroke:** Reduced blood flow to the brain can lead to a stroke.
* **Aortic aneurysm:** Weakening of the walls of the aorta, the body's largest artery.
### Diagnosis and Treatment
GCA is diagnosed based on a combination of symptoms, physical examination, and diagnostic tests. These tests may include:
* **Erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP):** Blood tests that measure inflammation in the body.
* **Temporal artery biopsy:** A small sample of the temporal artery is removed and examined under a microscope for signs of inflammation.
* **Imaging tests:** Ultrasound or MRI can be used to visualize the arteries and look for signs of inflammation.
Treatment for GCA typically involves high doses of corticosteroids, such as prednisone. These medications help to reduce inflammation and prevent complications. Treatment is usually long-term, and the dosage of corticosteroids may need to be adjusted over time.
> "Giant cell arteritis requires prompt diagnosis and treatment to prevent potentially devastating complications like vision loss and stroke."
**Table: Comparing Temporal Arteritis and Polymyalgia Rheumatica**
| Feature | Temporal Arteritis (GCA) | Polymyalgia Rheumatica (PMR) |
| --------------------- | -------------------------------------- | --------------------------------------- |
| Arteries Affected | Primarily arteries in the head (temporal) | Not primarily arterial |
| Head Ache | Common, often in the temples | Less common |
| Jaw Claudication | Common | Rare |
| Vision Problems | Common | Rare |
| Muscle Pain | Less prominent | Prominent, especially in shoulders/hips |
| Often Occur Together | Yes | Yes |
## 5. Sinus Infections: Pressure and Inflammation 🤧
Sinus infections, also known as sinusitis, occur when the sinuses, air-filled cavities in the skull, become inflamed and blocked. This can lead to a buildup of pressure and mucus, causing pain and discomfort. While sinus infections are typically not considered a serious condition, they can sometimes cause head aches and eye pain.
### How Sinus Infections Cause Headaches and Eye Pain
The sinuses are located near the eyes and forehead, so inflammation and pressure in the sinuses can radiate to these areas, causing:
* **Head ache:** Often a dull, aching pain in the forehead, temples, or around the eyes.
* **Eye pain:** Pain or pressure behind the eyes.
* **Facial pain:** Tenderness or pain when touching the face.
### Other Symptoms of Sinus Infections
In addition to head ache and eye pain, other symptoms of sinus infections may include:
* **Nasal congestion:** A stuffy or blocked nose.
* **Nasal discharge:** Thick, discolored mucus draining from the nose.
* **Postnasal drip:** Mucus dripping down the back of the throat.
* **Cough:** Often worse at night.
* **Fatigue:** Feeling tired and run down.
* **Fever:** A low-grade fever.
### Diagnosis and Treatment
Sinus infections are typically diagnosed based on symptoms and a physical examination. In some cases, a CT scan may be needed to confirm the diagnosis and rule out other conditions.
Treatment for sinus infections may include:
* **Decongestants:** Medications to help clear nasal congestion.
* **Nasal saline rinses:** Rinsing the nasal passages with saline solution to help clear mucus.
* **Pain relievers:** Over-the-counter pain relievers to relieve head ache and facial pain.
* **Antibiotics:** If the sinus infection is caused by bacteria, antibiotics may be prescribed.
### When to See a Doctor
Most sinus infections resolve on their own within a few weeks. However, if your symptoms are severe or persistent, or if you develop a fever or other complications, it's important to see a doctor.
**Table: Comparing Viral and Bacterial Sinus Infections**
| Feature | Viral Sinus Infection | Bacterial Sinus Infection |
| ---------------- | ---------------------------- | ------------------------------- |
| Cause | Virus | Bacteria |
| Duration | Typically less than 10 days | Often longer than 10 days |
| Severity | Usually milder | Can be more severe |
| Nasal Discharge | Clear or white | Thick, yellow or green |
| Fever | Less common | More common |
| Response to Antibiotics | No response | Responds to antibiotics |
## Conclusion: Listen to Your Body 👂
While stress and eye strain are common causes of head aches, it's important to be aware of the potential for more serious underlying conditions, especially when your head ache is accompanied by eye pain or visual disturbances. Recognizing the alarming signs discussed in this article – glaucoma, migraine with aura, optic neuritis, giant cell arteritis, and sinus infections – can help you seek timely medical attention and prevent potential complications.
Remember, this article is intended for informational purposes only and should not be considered medical advice. If you are experiencing persistent or severe head aches with eye pain, consult with a qualified healthcare professional for proper diagnosis and treatment. Your health is your most valuable asset, so prioritize it and listen to your body! 💖Share this content:

